What is length time bias?
What is length time bias, why is it important, how do you avoid it and how it differs from lead time bias.
Lead time bias and length time bias are epidemiological concepts in public health used to evaluate screening programmes, especially those for cancer.
What is length time bias?
To understand length time bias quickly, all you need to do is to answer this question: What kind of diseases are more likely to be detected by screening? A rapidly-growing tumour or a slow-growing one?
The answer: a slow growing one.
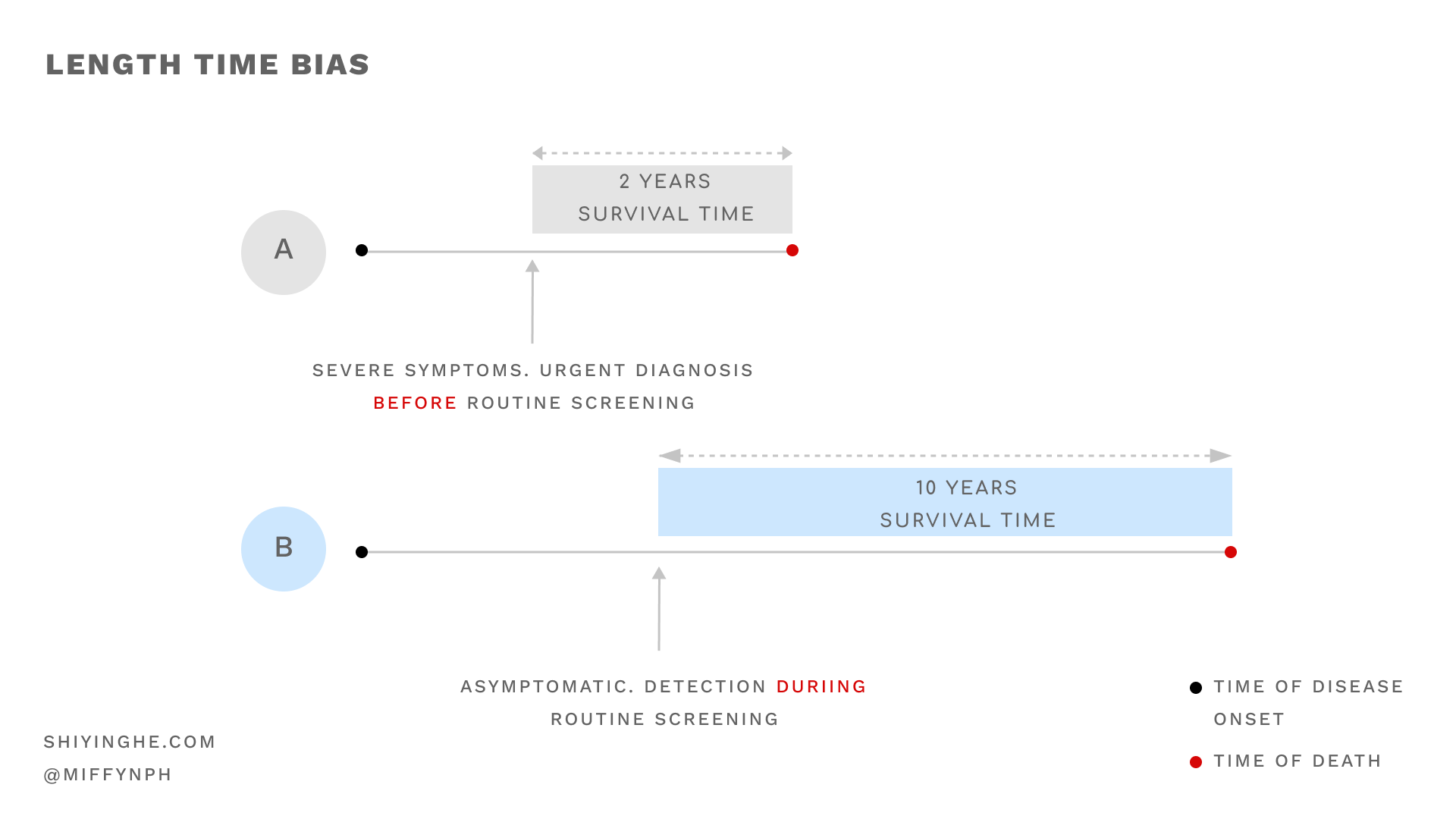
Rapidly-progressing diseases would often present severe symptoms that require immediate clinical attention. They are usually less likely to be diagnosed through screening.
On the other hand, slowly-progressing diseases often remain asymptomatic for a period of time. They are detectable through screening (because they have longer detectable pre-clinical phases) but their disease has not become severe enough to present symptoms yet.
Hence, patients with less severe diseases are more likely to have them detected during screening. And because the diseases are slow-progressing, these patients tend to have longer survival periods.
Why is length time bias important?
Length time bias leads us to think that it was the screening was responsible for higher survival rates. This becomes a problem when in actual fact, the survival rates were caused by the rate of disease progression, not the screening.
Another problem lies in the severe form of length time bias: overdiagnosis. This occurs when screening detects cancers that would otherwise not have exhibited clinical symptoms in a patient's lifetime. Examples of overdiagnosis include in-situ cancers that might never metastasize or present any symptoms. Detection of the disease might lead to unnecessary anxiety or even harmful operation procedures.
How to avoid length time bias?
The way to prevent length time and lead time biases are similar.
To prevent length time bias, we should not compare survival rates. Instead, we should examine the disease mortality rates in randomised controlled trials where the population of interest is randomly allocated to screening and non-screening groups. In the case of breast cancer, they are the mammography and control groups respectively.
Mortality rate per 1,000 population = total no. of deaths from breast cancer in a year/ estimated population with breast cancer in that year * 1000
Length time bias is present if:
- The mortality rate for patients of breast cancer is the same for screening and non-screening groups and;
- Those who were diagnosed during screening had more benign or slowly-progressing forms of the disease and;
- The study concludes that screening increases survival rates.
How is it different from lead time bias?
Check out the post on lead time bias here.
Conclusion
Length time bias occurs when patients with less severe diseases are more likely to have them detected during screening. Length time bias leads us to think that it was the screening was responsible for higher survival rates. This becomes a problem when the higher survival rates were caused by the rate of disease progression, not the screening. If not accounted for, this bias can result in the false conclusion that screening is able to prolong survival time.
We explore a related but distinct concept called lead time bias in a separate post here.
Sources
- Stephen W. Duffy, Iris D. Nagtegaal, Matthew Wallis, Fay H. Cafferty, Nehmat Houssami, Jane Warwick, Prue C. Allgood, Olive Kearins, Nancy Tappenden, Emma O'Sullivan, Gill Lawrence, Correcting for Lead Time and Length Bias in Estimating the Effect of Screen Detection on Cancer Survival, American Journal of Epidemiology, Volume 168, Issue 1, 1 July 2008, Pages 98–104, https://doi-org.libproxy1.nus.edu.sg/10.1093/aje/kwn120
- Webb, P., Bain, C., & Page, A. (2016). Essential Epidemiology: An Introduction for Students and Health Professionals (3rd ed.). Cambridge: Cambridge University Press. doi:10.1017/9781316275948
Stay updated on the best insights from public health professionals.