What is lead time bias?
What is lead time bias, why is it important, how do you avoid it and how it differs from length time bias.
Lead time bias and length time bias are concepts in epidemiology that are used to evaluate screening programmes, particularly in cancer screening.
When we conduct screening for diseases, we want to make sure that people do not waste time on a procedure that does not benefit them in any way. Screening should improve health outcomes, not lead to unnecessary anxiety or stress.
What is lead time bias?
To 'lead' is to be ahead or to go first. 'Lead time bias' happens when you detect a disease during a health screening procedure. This detection occurs earlier- before the usual diagnosis when the disease is symptomatic. The earlier a disease is diagnosed, the longer a patient will appear to survive. Lead time bias is present when this initial 'lead time' is not accounted for during the evaluation of the screening programme.
Let's take an example of two women. Woman A went for a routine breast cancer screening and was diagnosed with breast cancer at age 55. Woman B was diagnosed during a doctor's visit to investigate a sudden pain in her breasts at age 65.
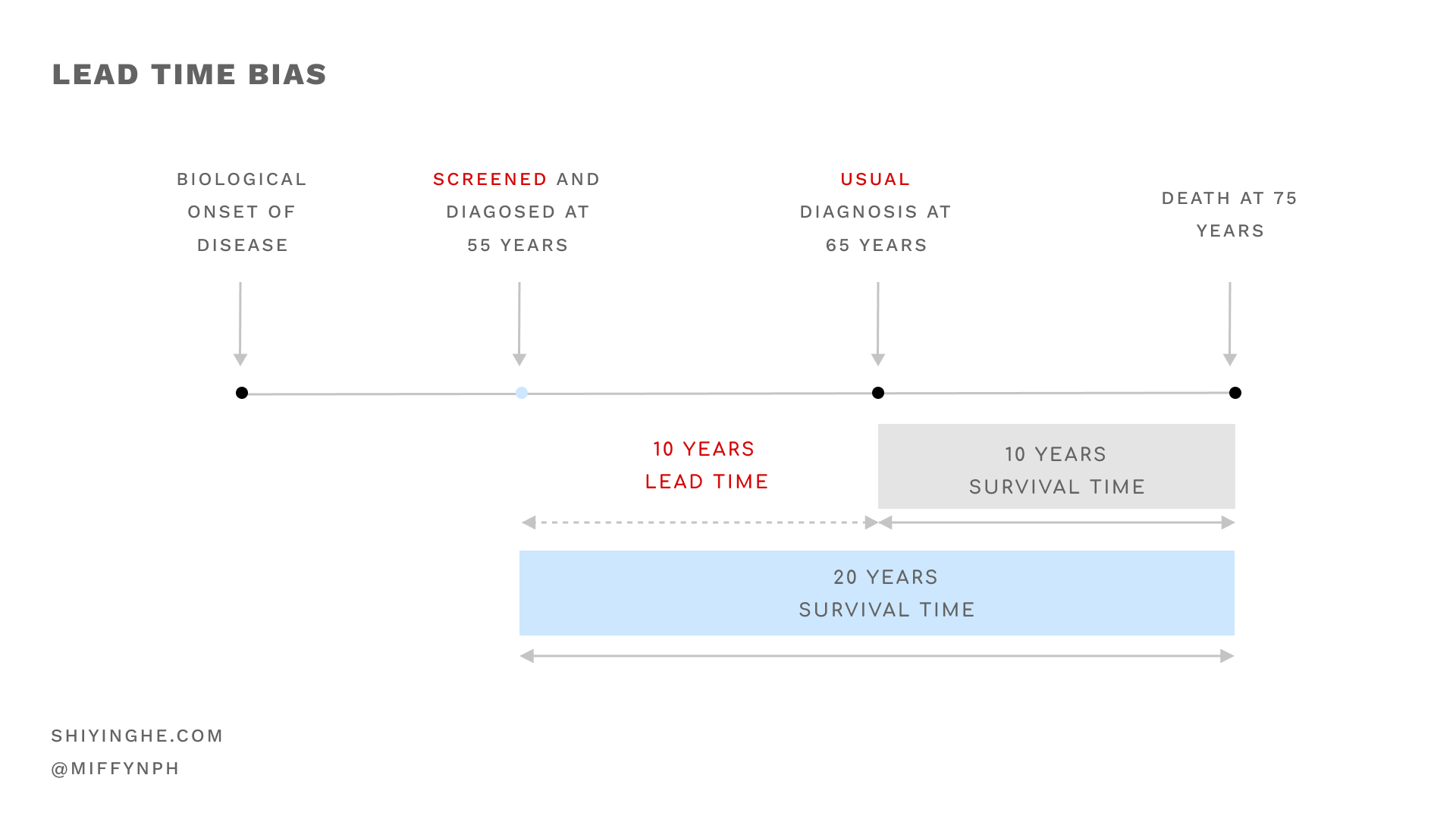
Looking at the above image, both women started developing the disease at a similar time. Both also died around the same time. If you compare both women's medical records, it seems like breast cancer screening has increased survival time for Woman A by 10 more years.
However, it might not be the screening that prolongs survival time. Instead, screening only lengthened the time period the person is considered a patient.
Why is lead time bias important?
If we disregard lead time bias, we might falsely conclude that screening increases survival rate, even if those screened vs unscreened experienced the same disease progression.
We might also overlook the fact that screening might do more harm than good. Woman A had spent 10 more years knowing about her disease. That's 10 more years of travelling to and fro the hospital and unnecessary anxiety.
How to avoid lead time bias?
The way to prevent lead and length time biases are similar.
To prevent lead time bias, we should not compare survival rates. Instead, we should examine the disease mortality rates in randomised controlled trials where the population of interest is randomly allocated to screening and non-screening groups. In the case of breast cancer, they are the mammography and control groups respectively.
Mortality rate per 1,000 population = total no. of deaths from breast cancer in a year/ estimated population with breast cancer in that year * 1000
Lead time bias is present if:
- The mortality rate for patients of breast cancer is the same for screening and non-screening groups AND;
- And the study concludes that screening increases survival rates.
How is it different from length time bias?
Check out the post on length time bias here.
Conclusion
'Lead time bias' occurs when a disease is detected during a health screening procedure, before the usual diagnosis when the disease is symptomatic. The earlier a disease is diagnosed, the longer a patient's survival time appears to be. Lead time bias is present when this initial 'lead time' is not accounted for during the evaluation of the screening programme and results in the false conclusion where screening is able to prolong survival time.
We explore a related but distinct concept called length time bias in a separate post here.
Sources:
- Stephen W. Duffy, Iris D. Nagtegaal, Matthew Wallis, Fay H. Cafferty, Nehmat Houssami, Jane Warwick, Prue C. Allgood, Olive Kearins, Nancy Tappenden, Emma O'Sullivan, Gill Lawrence, Correcting for Lead Time and Length Bias in Estimating the Effect of Screen Detection on Cancer Survival, American Journal of Epidemiology, Volume 168, Issue 1, 1 July 2008, Pages 98–104, https://doi-org.libproxy1.nus.edu.sg/10.1093/aje/kwn120
- Webb, P., Bain, C., & Page, A. (2016). Essential Epidemiology: An Introduction for Students and Health Professionals (3rd ed.). Cambridge: Cambridge University Press. doi:10.1017/9781316275948
Stay updated on the best insights from public health professionals.