Global Governance of Vaccine Equity: A Literature Review
A literature review on the current state of how pandemimc vaccine equity is governed at the global level.
Done by: He Shiying (September 2021)
Introduction
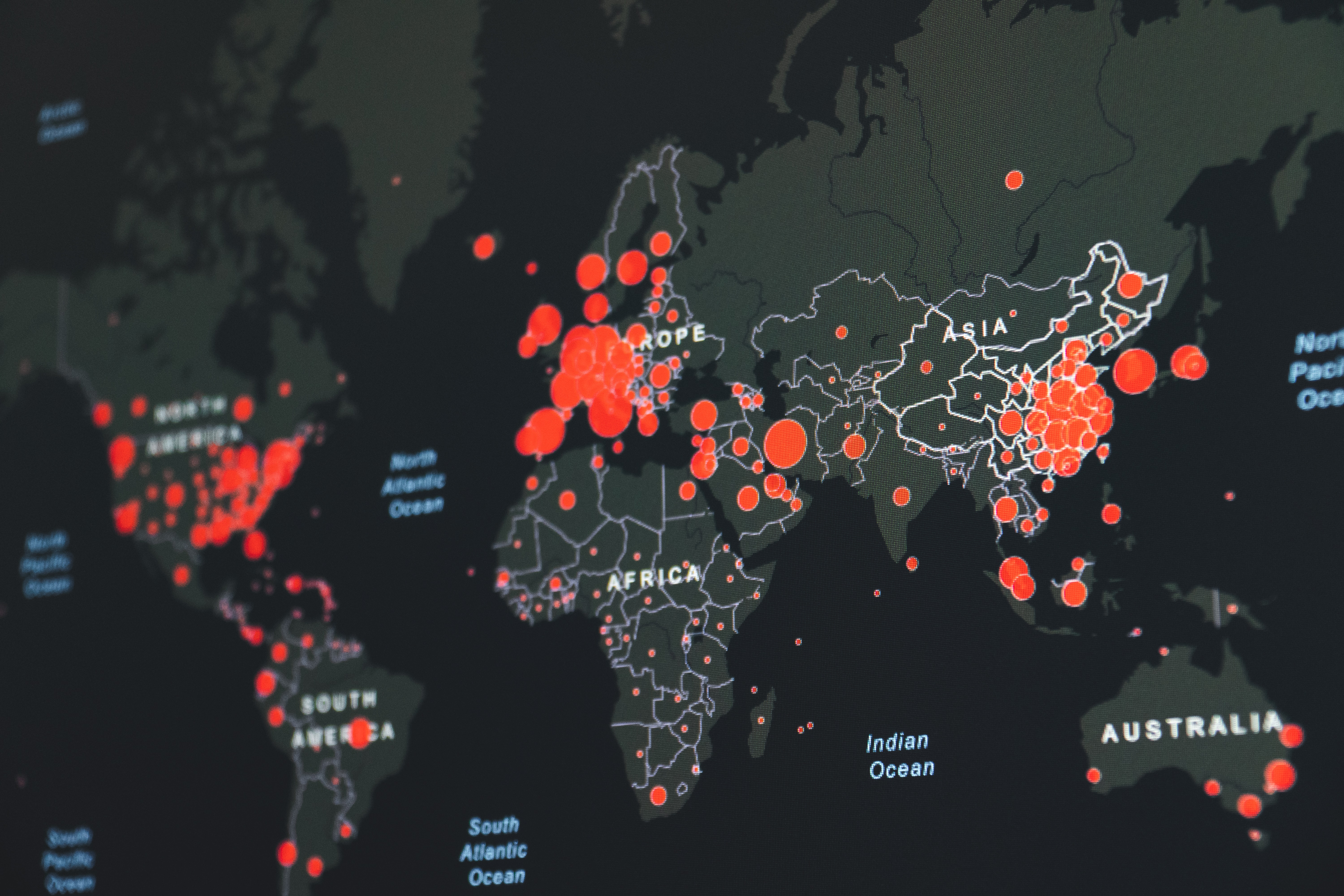
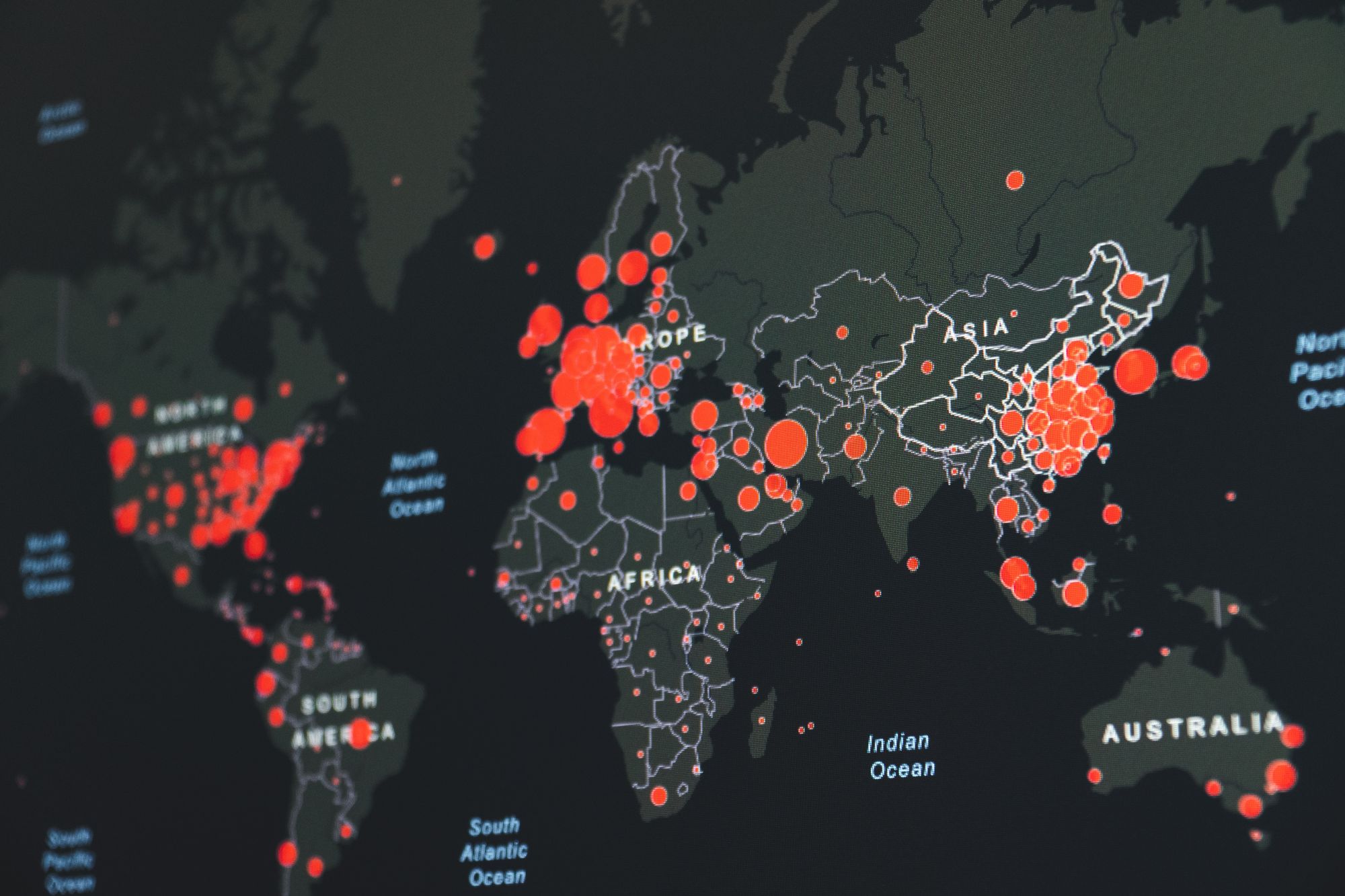
The COVID-19 pandemic has wrought devastating economic and social disruption worldwide, with tens of millions at risk of slipping into extreme poverty (Chriscaden, 2020). The pandemic has brought about severe crises across public health, employment and labour, food security sectors, and its impacts are worst felt by the poor (Chriscaden, 2020). Vaccination presents the most important opportunity for the world to overcome this ordeal. However, as of 23 September 2021, just 10% of people in LMICs are fully vaccinated (Maxmen, 2021). The numbers are more dismal in low-income countries, with less than 1% fully vaccinated (Maxmen, 2021). This gap between wealthy and poor countries will continue to widen as booster shots become increasingly in demand. It is crucial to address a global health issue such as ensuring vaccine equity- particularly how COVID-19 vaccine equity is governed on the global stage. The pandemic is a global health challenge that can only be overcome collectively- and vaccines offer the most potent tool to do so. As such, this literature review is an attempt to synthesize current literature discussing the global governance of vaccine equity, with a focus on pandemic vaccines.
This review will outline current international laws governing vaccine equity, the gaps in global governance of vaccine equity, the lessons gained from the 2009-H1N1 pandemic, COVID-19 Vaccines Global Access’s (COVAX) effectiveness and the possible next steps to improve current global governance efforts. This review has found that while substantial literature exists expounding on the ideal governmental structures required to attain vaccine equity, further work is required to evaluate the practicality and effectiveness of such lessons and recommendations in actual policies implemented.
International Law Governing Vaccine Equity
When it comes to ensuring vaccine equity, the literature frequently draws on international human right norms. There were repeated references to the World Health Organization (WHO) Constitution, the International Covenant on Economic, Social and Cultural Rights (ICESCR), International Health Regulations (IHR) as well as the Universal Declaration of Human Rights (UDHR) (Gostin et al., 2020; Labonté & Schrecker, 2007; A. Phelan, 2020; A. L. Phelan, Katz, et al., 2020). For example, the right to health is first expressed in the WHO Constitution, stating that “[t]he enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being without distinction of race, religion, political belief, economic or social condition.” (A. Phelan, 2020). The right to health was also subsequently enshrined in the Universal Declaration of Human Rights (UDHR), which has been argued to be part of customary international law (A. L. Phelan, Eccleston-Turner, et al., 2020).
There is also much discussion about the obligation all states have to collectively realise the right to health, with pandemics being a pertinent example. For instance, Phelan argues that the "full realisation of the right to health globally" is intrinsically contingent upon international cooperation, especially for infectious diseases that are easily transmissible across state borders (Phelan, 2020). Further, as per the IHR, "states have obligations to prevent, detect, respond, and control the spread of international public health threats, including obligations to provide international assistance and cooperation" (A. Phelan, 2020).
Yet, specific the international legal instruments currently in place to ensure vaccine equity appear to be weak. The Nagoya Protocol is one example. While it obliges developing countries to provide access to biological samples to developed countries to develop vaccines and drugs, there are no equal obligations imposed on developed countries to provide assistance, cooperation, or benefit sharing in the form of developed vaccines (A. Phelan, 2020).
Gaps in Global Governance
The other existing instrument is called the Pandemic Influenza Preparedness (PIP) Framework, which had been introduced by the WHO since the H1N1 pandemic (Turner, 2016). It is the only international legal instrument that oversees equal distribution of vaccines before the COVID-19 pandemic. In enabling the WHO to manage a stockpile of 150 million vaccines, this framework aims to enlarge access to pandemic influenza vaccines (McAdams et al., 2020; Turner, 2016). However, this instrument has seen limited effectiveness because only 2 out of 25 influenza vaccine manufacturers have come on board, and failed to make the full donation commitments (Turner, 2016). Critics have also argued that the framework would have limited impact firstly because similar measures have been tried and tested outside the framework with limited success at expanding access to vaccines. Secondly, it does not alter any of the existing market-based economy that drives vaccine production and procurement (Turner, 2016). Thirdly, since the PIP Framework’s distribution processes are determined based on countries' public health needs and risks, the framework is rendered unhelpful because an actual pandemic will see a limited vaccine supply with equally urgent needs across countries, making distribution based on need and risk difficult (A. L. Phelan, Eccleston-Turner, et al., 2020). Fourthly, the framework is specialised for influenza vaccines only. This means that for non-influenza pathogens like SARS-CoV-2, which is responsible for the COVID-19 pandemic, states are left without an international framework to look to for guidance.
The existing vaccine procurement mechanisms also structurally promote vaccine nationalism. There are two main ways by which countries can procure or receive their vaccines. Self-procurement, also known as bilateral agreements to directly purchase from manufacturers, is the fastest and most efficient way to procure vaccines (Turner, 2016). However, it is expensive – in terms of finances and technical knowledge. Hence, HICs are more likely to be able to self-procure vaccines. States that are unable to self-procure vaccines may receive them as donations from International Organisations (IOs) such as GAVI Alliance, WHO and UNICEF (Turner, 2016). These IOs may receive donations from manufacturers and states or act as a procurement agent by purchasing vaccines directly from manufacturers. During the H1N1 and COVID-19 pandemic, we see HICs self-procuring via Advanced Purchase Agreements (APAs), also known as sleeping contracts between a government and a vaccine manufacturer (Eccleston-Turner & Upton, 2021; McAdams et al., 2020). APAs allow governments to reserve doses of a vaccine for diseases that have not even arisen. In the previous 2009-H1N1 pandemic, there was already evidence of vaccine nationalism, for vaccines were the only means of preventing infection of a rapidly-transmissive virus (Fidler, 2010). This was evident in the 2009-H1n1 pandemic in two ways. First, developed countries had placed advanced orders for the 2009-H1N1 vaccine- reserving majority of the globe's manufacturing capacity for themselves (Fidler, 2010; Turner, 2016). The WHO and the UN had to appeal to countries and manufacturers for monetary donations to purchase vaccines to meet the needs in developing countries- which still left them with limited supplies (Fidler, 2010). As such, we learn that APAs are ineffective at securing sufficient levels of access to vaccines for developing states.
Learning from the 2009-H1N1 pandemic
During the H1N1 pandemic, a mere 12.3% of all influenza vaccines were donated, compared to 59.4% via self-procurement (Turner, 2016). To understand the extent of reliance on donations, the African region derived 94.5% of its vaccines from these donations, and for the South-East Asian region, the number was at 91.2% (Turner, 2016). It was evident that developing states were dependent on donations, which is dangerously prone to vaccine nationalism (Turner, 2016). To illustrate, the WHO had distributed 40% of the doses for developing states at least three months after developed states received theirs, when states were already entering a 'post-pandemic phase' (Turner, 2016). This delay resulted in 7000 deaths, primarily occurring in developing states- a number that will only inflate in a more severe pandemic (Turner, 2016).
There are however, redeeming points about the pandemic. Unlike other pieces of literature that had been heavy on the criticism, Abelin et al.'s piece had been generous in their praises for the vaccine industry's response during the H1N1 pandemic. The authors argue that the vaccine manufacturers, thanks to longstanding commitment to pandemic preparations the past decade, was able to churn out "significant quantities of safe and effective vaccines" a mere three months after the declaration of the pandemic (Abelin et al., 2011). The authors also praised the efficient collaboration that occurred between "between global health authorities, scientists and manufacturers" to facilitate what they described as "the most comprehensive pandemic response undertaken" (Abelin et al., 2011). The glowing response in contradiction to other pieces on the pandemic could be because of the authors’ positions in The International Federation of Pharmaceutical Manufacturers and Associations International Vaccine Supply taskforce, which requires good diplomatic skill to navigate interests of all parties (Abelin et al., 2011).
COVAX’s Effectiveness
Eccleston-Turner and Upton's paper is the first thorough analysis of COVAX and whether it has met its aims of guaranteeing equitable access to COVID-19 vaccines in LMICs. Sure enough, it echoes previous literature in stating that while equitable access to the vaccines remains a priority, evidence from past pandemics predict that access will continue to be limited in developing countries (Eccleston-Turner & Upton, 2021; A. L. Phelan, Eccleston-Turner, et al., 2020; Turner, 2016). Fortunately, COVAX Facility's at-risk funding strategy has been successful specifically in accelerating COVID-19 vaccine development. It has managed to fast-track and scale at-risk investments in vaccine research and development as well as to expedite the production of doses even before clinical efficacy has been established (Eccleston-Turner & Upton, 2021). COVAX pillar–funded AstraZeneca/Oxford has also received regulatory approval- a successful portfolio candidate because it is viable for distribution in LMICs given its capacity to be manufactured rapidly globally, more easily stored compared to the mRNA vaccines and is significantly. This arm of COVAX has truly successfully resulted in the most rapid development of a vaccine for a new pathogen. (Eccleston-Turner and Upton, 2021).
However, the success has not transferred over into its role as a procurement tool for LMICs. COVAX's success is limited by widespread prevalence of vaccine nationalism, where wealthy nations' participation in bilateral advance purchase agreements put them in direct competition with the COVAX Facility for vaccine doses (Dyer, 2020; Eccleston-Turner & Upton, 2021; Eyawo & Viens, 2020). The COVAX Facility's efforts are undermined by bilateral advance purchase agreements because they increase global competition for a limited supply of vaccines.
Recommendations for steps forward
Several papers talk about leveraging on crisis as catalyst- that COVID-19 presents an opportunity to reinforce core principles and goals of global health governance, particularly the principle of equity to ensure equitable access to vaccines.
First, IOs can look to alternative funding arrangements rather than relying on the goodwill of donors. There is currently an abundance of untapped funding fund in sovereign wealth funds, insurance companies and more that can be used to address health crises- including the COVID-19 pandemic (Kickbusch et al., 2018). However, it is the mobilisation of these resources that is difficult. Vaccine equity falls under the broad umbrella of global health equity- a domain that requires long-term, sustainable financial investment. Annual funding for global health, including vaccine equity is pegged to increase to US$274-$371 billion by 2030 (Kickbusch et al., 2018). The scale of the vaccine equity problem, just like many other global health issues, is too large to be resolved through charitable capital alone. This financial need requires the critical participation of the private sector. However, current financial markets lack the necessary structures to facilitate the needed sustainable investment in global health to provide returns to investors. Hence, IOs can look to filling this gap in order to ensure long-term sustainable financial returns on goals such as vaccine equity (Kickbusch et al., 2018)
Second, IOs can reconfigure APAs to the international community’s advantage. McAdams et al. acknowledges that bilateral deals such as APAs are inevitable. What the international community needs to do is to "configure these deals to also benefit the new COVAX” and incentivise wealthy countries to make bilateral deals that have positive deals for everyone else (McAdams et al., 2020). Two ways this could be done is to increase the fungibility of investments in vaccine candidates and to ensure supply chain harmonisation (McAdams et al., 2020).
Conclusion
This literature review has outlined the current international laws governing vaccine equity, the gaps in global governance of vaccine equity, the lessons gained from the 2009-H1N1 pandemic, COVID-19 Vaccines Global Access’s (COVAX) effectiveness and the possible next steps to improve current global governance efforts.
This review has also found that there is a dearth of studies examining the effectiveness of COVAX since its inception. There is also a lack of studies examining how lessons from the 2009-H1N1 pandemic has been incorporated into later funding mechanisms and international regulations, including COVAX. There is also little literature investigating the incentives in place that fund pharmaceutical R&D during a global public health emergency, and the implications of such in future pandemics. This could be because the contractual agreements between governments, non-governmental organisations and the pharmaceutical industries are opaque to the public. Much of the literature also gloss over the roles that stakeholders such as states, IOs, non-profit organisations, manufacturers and health authorities play in the global governance of vaccine equity.
In sum, while there is much existing literature examining the ideal governmental structures required to attain vaccine equity, further work is required to evaluate the practicality and effectiveness of such lessons and recommendations in actual policies implemented.
Word count: 2000 (Excluding citations).
References
Abelin, A., Colegate, T., Gardner, S., Hehme, N., & Palache, A. (2011). Lessons from pandemic influenza A(H1N1): The research-based vaccine industry’s perspective. Vaccine, 29(6), 1135–1138. https://doi.org/10.1016/j.vaccine.2010.11.042
Chriscaden, K. (2020, October). Impact of COVID-19 on people’s livelihoods, their health and our food systems. http://www.who.int/news/item/13-10-2020-impact-of-covid-19-on-people's-livelihoods-their-health-and-our-food-systems
Dyer, O. (2020). Covid-19: Many poor countries will see almost no vaccine next year, aid groups warn. BMJ, m4809. https://doi.org/10.1136/bmj.m4809
Eccleston-Turner, M., & Upton, H. (2021). International Collaboration to Ensure Equitable Access to Vaccines for COVID-19: The ACT-Accelerator and the COVAX Facility. The Milbank Quarterly, 99(2), 426–449. https://doi.org/10.1111/1468-0009.12503
Eyawo, O., & Viens, A. M. (2020). Rethinking the Central Role of Equity in the Global Governance of Pandemic Response. Journal of Bioethical Inquiry, 17(4), 549–553. https://doi.org/10.1007/s11673-020-10001-2
Fidler, D. P. (2010). Negotiating Equitable Access to Influenza Vaccines: Global Health Diplomacy and the Controversies Surrounding Avian Influenza H5N1 and Pandemic Influenza H1N1. PLOS Medicine, 7(5), e1000247. https://doi.org/10.1371/journal.pmed.1000247
Gostin, L. O., Karim, S. A., & Meier, B. M. (2020). Facilitating Access to a COVID-19 Vaccine through Global Health Law. Journal of Law, Medicine & Ethics, 48(3), 622–626. https://doi.org/10.1177/1073110520958892
Kickbusch, I., Krech, R., Franz, C., & Wells, N. (2018). Banking for health: Opportunities in cooperation between banking and health applying innovation from other sectors. BMJ Global Health, 3(Suppl 1), e000598. https://doi.org/10.1136/bmjgh-2017-000598
Labonté, R., & Schrecker, T. (2007). Globalization and social determinants of health: Promoting health equity in global governance (part 3 of 3). Globalization and Health, 3(1), 7. https://doi.org/10.1186/1744-8603-3-7
Maxmen, A. (2021). The fight to manufacture COVID vaccines in lower-income countries. Nature, 597(7877), 455–457. https://doi.org/10.1038/d41586-021-02383-z
McAdams, D., McDade, K. K., Ogbuoji, O., Johnson, M., Dixit, S., & Yamey, G. (2020). Incentivising wealthy nations to participate in the COVID-19 Vaccine Global Access Facility (COVAX): A game theory perspective. BMJ Global Health, 5(11), e003627. https://doi.org/10.1136/bmjgh-2020-003627
Phelan, A. (2020). Human Rights Implications of Pathogen Sharing and Technology Transfer. In S. F. Halabi & R. Katz (Eds.), Viral Sovereignty and Technology Transfer (1st ed., pp. 120–134). Cambridge University Press. https://doi.org/10.1017/9781108676076.009
Phelan, A. L., Eccleston-Turner, M., Rourke, M., Maleche, A., & Wang, C. (2020). Legal agreements: Barriers and enablers to global equitable COVID-19 vaccine access. The Lancet, 396(10254), 800–802. https://doi.org/10.1016/S0140-6736(20)31873-0
Phelan, A. L., Katz, R., & Gostin, L. O. (2020). The Novel Coronavirus Originating in Wuhan, China: Challenges for Global Health Governance. JAMA. https://doi.org/10.1001/jama.2020.1097
Turner, M. (2016). Vaccine procurement during an influenza pandemic and the role of Advance Purchase Agreements: Lessons from 2009-H1N1. Global Public Health, 11(3), 322–335. https://doi.org/10.1080/17441692.2015.1043743
Stay updated on the best insights from public health professionals.